Research
Mitochondrial ALDHs
The ALDH (aldehyde dehydrogenase) family of enzymes plays a critical role in detoxifying harmful aldehydes. These toxic compounds can originate from various sources, including cigarette smoke, alcohol consumption, exposure to formaldehyde, and internal metabolic processes such as lipid peroxidation and amino acid metabolism. In humans, the ALDH family consists of 19 distinct isozymes, each responsible for metabolizing specific substrates. Many of these isozymes have been linked to human diseases, and known mutations in the population can reduce their catalytic functions, leading to the accumulation of toxic aldehydes.
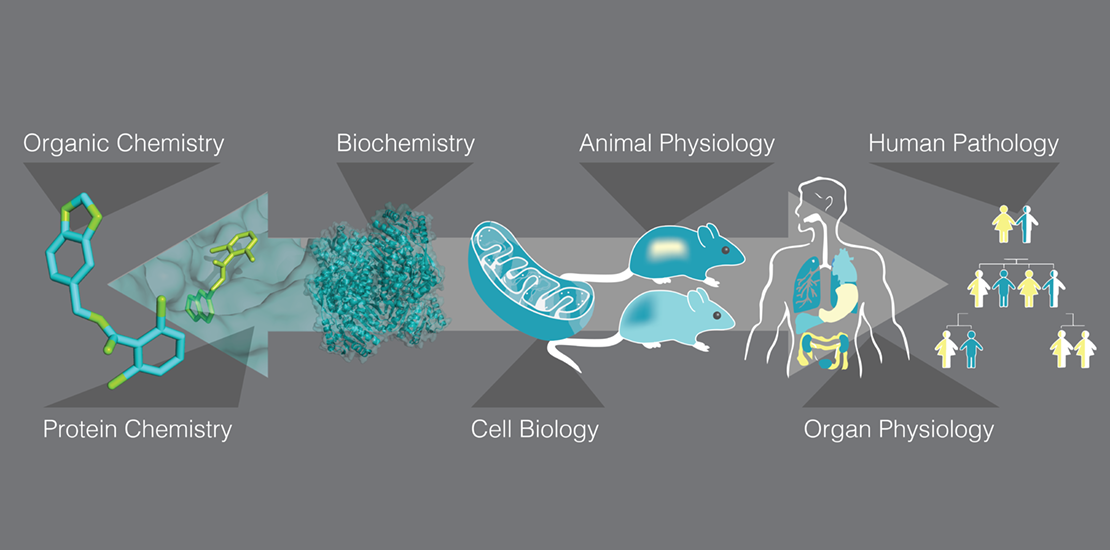
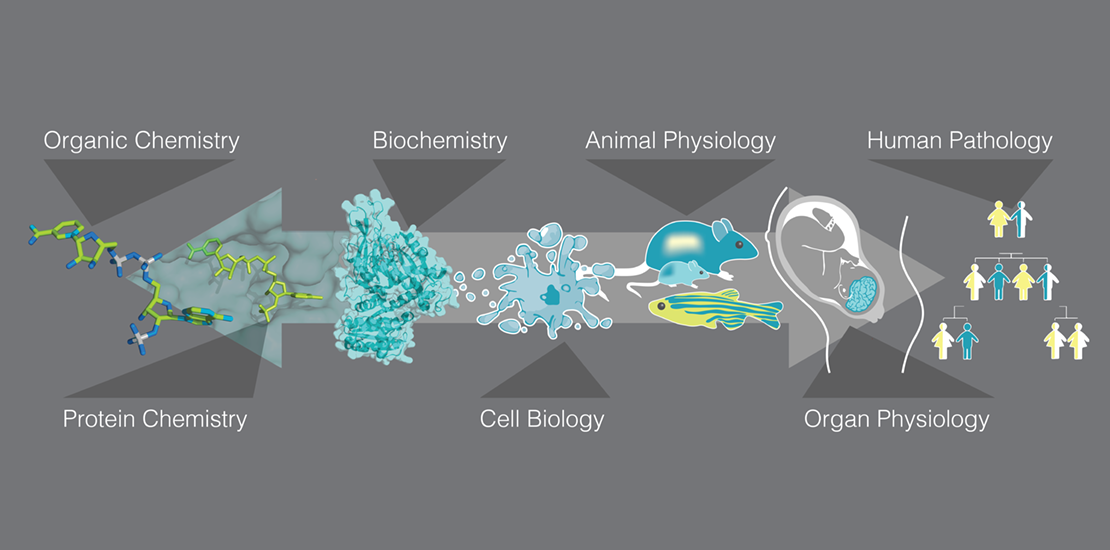
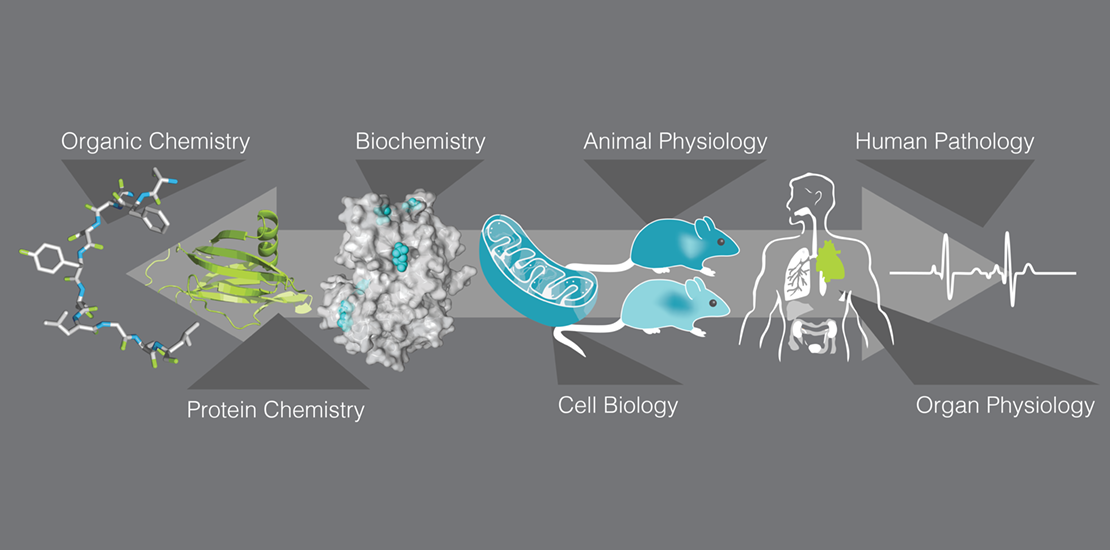
Our lab is dedicated to developing isozyme-specific small molecule modulators, enabling researchers to differentiate the functions of various ALDH isozymes. These modulators may prove beneficial in treating diseases associated with mutations in ALDH enzymes. Since mitochondria play a major role in human health, not only as the so-called ‘powerhouse of the cell’ producing ATP, but also as a hub in neutralizing damaging aldehydes, our research efforts are focused on the six mitochondrial ALDHs and currently on ALDH1, ALDH1B1, and ALDH4A1.
The most common human enzymopathy is due to a mutation in the mitochondrial ALDH2, afflicting about 0.7 billion people of East Asian descent. This ALDH2 causes facial flushing upon alcohol consumption, and while this mutation was considered benign, our activators for ALDH2 have shown promise in improving outcomes across various models of human diseases, including myocardial infarction, inflammatory pain, radiation dermatitis, stroke, and Parkinson’s disease. Epidemiological studies have further supported the role of ALDH2 in these conditions.
We discovered that mitochondrial aldehyde dehydrogenase 2 (ALDH2) is crucial for cell survival under oxidative stress and developed novel ALDH2 activators, termed Aldas (for ALDH activators). The work was first reported in Science (2008); since then, more than 100 independent studies have shown the benefit of Aldas in a variety of human diseases. Aldas correct the structural mutation in ALDH2 that affects around 0.7 billion East Asians, representing a new class of drugs that act as molecular chaperones, as highlighted in Nature Structure and Molecular Biology (2010). Our research contributed to the founding of ALDEA Pharma in 2011 with Dr. Che-Hong Chen, a senior scientist in our lab, and its patents were later licensed to Foresee Pharmaceuticals (currently in phase II studies in two indications). We also established STAR, an international research organization focused on ALDH2 enzymopathy. Given that defense against oxidative stress is crucial for cell survival, we continue to explore the benefits of activating various ALDH enzymes in diverse diseases, including Fanconi Anemia, neurodegenerative diseases, and radiation-related conditions. For instance, we have utilized a small molecule to ‘hijack’ ALDH3A1, allowing it to metabolize the substrate of the mutated ALDH2 (PNAS, 2015), in Alzheimer’s disease (Acta Neuropathol Commun. 2019), in other neurodegenerative diseases (Front Aging Neurosci. 2023), and in cancer (Life, 2022).
Our interest in mitochondrial functions has led us to investigate other mitochondrial ALDHs. For instance, through in vitro studies and mouse models, we discovered that variants of ALDH4A1 are linked to the ultra-rare disease, hyperprolinemia type 2 (HPII; submitted for publication), as well as to more common conditions, such as inflammatory bowel disease (IBD; in preparation) and Alzheimer’s disease. Our current efforts focus on generating small molecules that will increase ALDH4A1 activity.
We are also examining the role of mitochondrial ALDH1B1, a highly homologous enzyme to ALDH2. By analyzing human genetic data and concentrating on common variants in ALDH1B1, we have identified its significant role as a mitochondrial ALDH (this work has also been submitted for publication).
Mitochondrial Dynamics
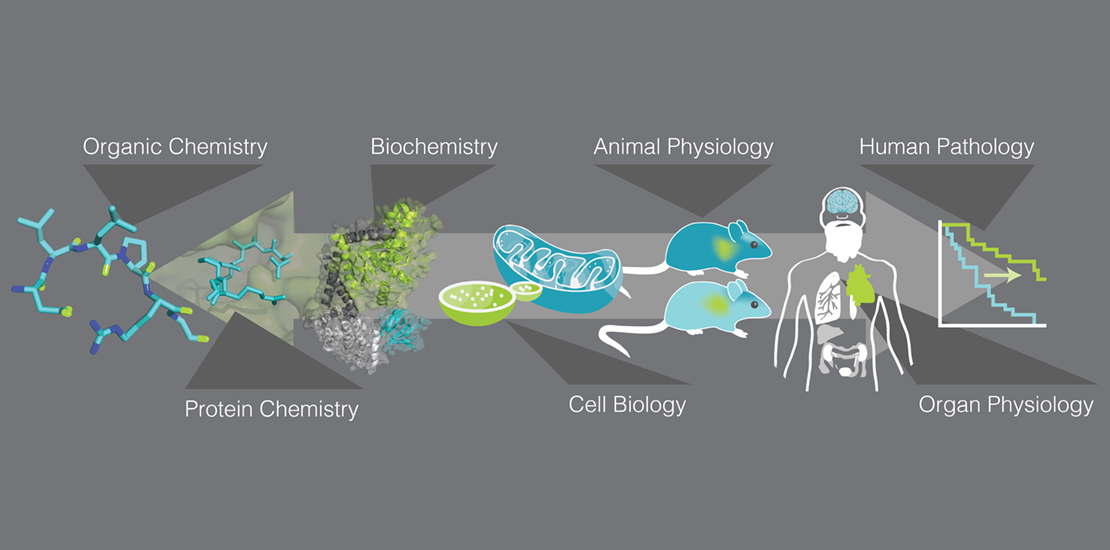
Mitochondria, a dynamic network of organelles, play a major role in many cellular processes – from generating ATP and many building blocks, to coordinating apoptosis and anti-viral response, and by participating in the synthesis of important signaling molecules, like steroids, neurotransmitters, cortisol, melatonin, and heme. Therefore, the maintaining functioning of the mitochondria is important to human health. We and others have found that many human pathologies are associated with excessive mitochondrial fragmentation. We were the first to demonstrate that the binding of the cytosolic dynamin-related protein 1 (Drp1) to the mitochondrial surface protein, Fis1, promotes this pathological excessive fission. We then used a rational approach to inhibit this protein/protein interaction; we have identified P110, a heptapeptide that selectively inhibits this pathological interaction, without affecting the physiological role of Drp1 in regulating mitochondrial dynamics (JCS, 2013).
Systemic and sustained P110 treatment in various neurodegenerative diseases using patient-derived cells and mouse models showed substantial benefits in Parkinson’s disease (JCS, 2013), Huntington’s disease (JCI, 2013), in cardiac ischemia (JAHA, 2013), in amyotrophic lateral sclerosis (ALS; EMBO Mol Med, 2018), and in Alzheimer’s disease (Oncotarget, 2017). The benefits were associated with improved mitochondrial function, reduced protein aggregation, reduced cell death, behavioral improvement, and longer lifespan in these models. Additionally, P110 has been independently tested by other laboratories in a variety of human diseases, demonstrating efficacy in conditions such as inflammatory bowel disease, stroke, and kidney disease, among others.
Most recently, we focused on generating small molecules that selectively inhibit pathological mitochondrial fission. Our first small molecule inhibitor, SC9 (Nature Commun, 2023), targets Drp1 by binding to it and selectively preventing its interaction with Fis1. A second inhibitor, SP11, is a small molecule that inhibits the dimerization of Fis1, a process essential for Drp1 binding and the subsequent pathological fission of mitochondria (Nature Commun, 2025). The rationale search for this inhibitor is described in the 2025 publication, and its ability in vivo is currently under investigation in models of mitochondrial pathological fission.
G6PD
Glucose-6-phosphate dehydrogenase (G6PD) is a rate-limiting enzyme in the pentose phosphate pathway, responsible for generating NADPH and reduced glutathione (GSH). This enzyme plays a vital role in maintaining redox balance and managing oxidative stress, particularly in erythrocytes. Over 400 million people globally are affected by G6PD deficiency, which arises from a single amino acid variant in the enzyme. There are more than 160 known variants, leading to a wide range of symptoms, from chronic non-spherocytic hemolytic anemia to minimal clinical manifestations (Cell Report, 2017; Matters, 2017). These variants can influence the enzyme’s catalytic activity, stability, and oligomeric state (G6PD typically exists as a dimer of dimers).
We conducted a high-throughput screen to identify small molecules that can correct specific G6PD mutations by enhancing the catalytic activity or stability of the mutant enzyme. We identified AG1, a small molecule, that increases the catalytic activity of wildtype as well as several common human mutants (Nature Commun, 2018). Our medicinal chemistry efforts (ChemMedChem, 2019) and guidance from modeling (JBC, 2022) and crystallographic studies (PNAS, 2021) help optimize the compounds that increase the stability and activity of G6PD in vitro, in cell cultures, and in vivo models.
In addition to focusing on how G6PD variants contribute to hemolytic anemia, our recent efforts focus on the role of G6PD deficiency in other chronic diseases. Our studies suggest that in addition to its role in enhancing the redox potential of cells, which is crucial for overall human health, G6PD may have a non-catalytic role, via selective protein-protein interactions. Although this work is still in its early stages, there is potential for developing new therapeutic strategies for common human diseases through drugs that enhance the stability and protein-protein interactions of G6PD.
PKC
The PKC family of enzymes consists of a diverse group of proteins that play crucial roles in regulating cellular processes such as proliferation, apoptosis, and necrosis. Our laboratory’s initial contribution to this field involved the development of isozyme-specific modulators, which enabled researchers to differentiate the functions of individual PKC isozymes. Unlike many PKC inhibitors, our rationally designed short peptide regulators act as highly selective inhibitors of protein/protein interactions. Our work led, for example, to the identification of opposing effects of PKCδ and PKCε within mitochondria, particularly in the context of ischemic heart disease (PNAS, 1999; Circ Res, 2000; PNAS, 2001).
Given that each PKC isozyme phosphorylates multiple protein substrates, we next aimed to clarify the role of individual phosphorylation events. To achieve this, we designed peptide inhibitors that selectively inhibit the phosphorylation of one substrate at a time. Our findings demonstrated that simultaneous phosphorylation events mediated by the same protein kinase can produce either similar or opposing effects, highlighting the complexities of signal transduction regulation (JACS, 2016; Angew Chem Int Ed Engl. 2016). This research provides new insights into the orchestration of signaling pathways in both healthy and disease states.
Most recently, we discovered that the phosphorylation of cardiac troponin I (cTnI) during ischemia exposes a non-canonical role of this cytoskeletal protein; cTnI enters the mitochondria where it interacts with and inhibits ATP synthase (complex V). Peptide 888 that we have rationally designed inhibits post-ischemia and reperfusion injury (Pharmaceuticals, 2022; Nature Cardiovascular Res, 2024)
Our investigations focused on how protein-protein interactions govern cell signaling (Science, 1995). By employing rational approaches, we identified short peptide inhibitors that interfere with intracellular protein-protein interactions, influencing signal transduction under normal and pathological conditions (outlined in Nature Biotechnology, 1998). This work has led to the discovery of highly selective PKC inhibitors and activators, which are crucial for understanding the enzymatic roles in various cellular responses. Importantly, our peptide regulators have shown therapeutic potential in animal models of human diseases, including myocardial infarction and heart failure, as noted in Nature Review Drug Discovery (2013). A phase IIa clinical study revealed that one of our peptide inhibitors effectively reduced cardiac damage in patients with myocardial infarction (Circulation, 2008). This research supported the co-founding of KAI Pharmaceuticals in 2002 with Dr. Leon Chen, a graduate student from our lab; the company was acquired by Amgen in 2012, with one of its drugs subsequently approved in Europe, the USA, and Japan.